When migraine strikes

Did you know that this kind of headache is the third most common disorder in the world, and one of the most debilitating? Here’s what you should know.
It’s not all in your head
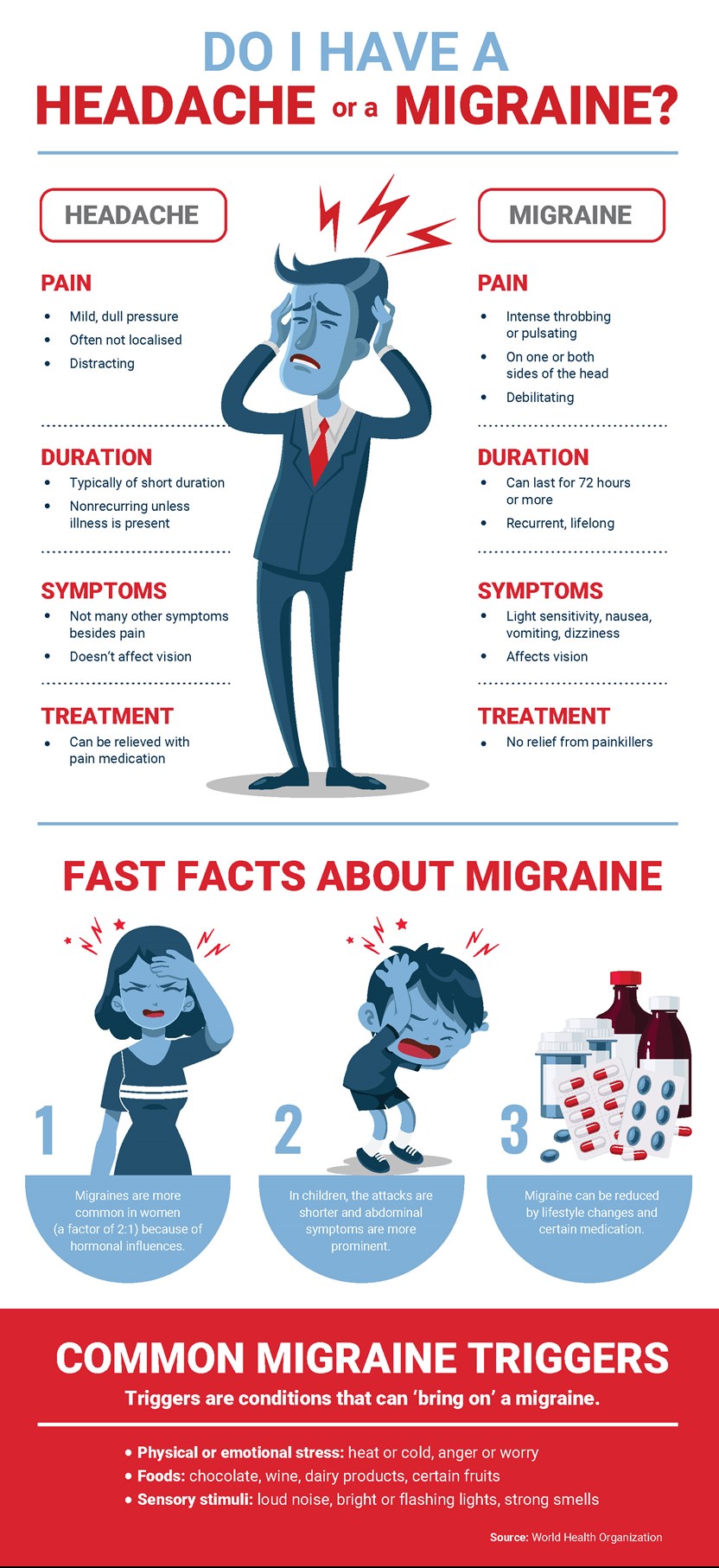
Migraine affects one in seven people. This is more than the number of people affected by diabetes, epilepsy and asthma combined. Some migraines are mild. Others are so severe that the World Health Organization (WHO) classifies them as among the most disabling illnesses.
Yet migraines tend to go undiagnosed and undertreated in at least 50% of patients. This is partly due to a lack of understanding of what migraine is, and how drastically it can affect people’s lives.
Identifying migraines
The WHO describes a migraine as a primary headache disorder (the headache is the condition itself, not a symptom of another condition) characterised by recurring attacks. A variety of symptoms differentiate migraine from other types of headaches, says Dr Kaushik Ranchod, a neurologist at Life Fourways Hospital in Johannesburg. He explains that migraine attacks typically progress through four phases:
- Phase one: the prodrome. Symptoms may include excessive yawning, neck stiffness, irritability and food cravings
- Phase two: aura. This presents as visual symptoms (bright shapes or objects, for example), auditory symptoms (such as noises and music), or sensory symptoms (for instance burning, pain or numbness)
- Phase three: headache. Usually unilateral (one-sided) and throbbing. Its intensity increases over time, and it’s often associated with nausea, and light and sound hypersensitivity.
- Phase four: the postdrome. The headache subsides. The patient feels physically and mentally drained.
To diagnose a migraine, Dr Ranchod would examine the patient and take their history. Based on the type of migraine identified, he would then create a suitable treatment plan. 
Treatment options
‘Migraines cannot be cured, but they can be managed,’ says Michelle Reddy, a clinical pharmacist at Life Groenkloof Hospital in Pretoria. Different medications are prescribed based on the severity and frequency of attacks. For mild to moderate migraines, these include paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs). For more severe cases, opioids or triptans could be more suitable.
However, all of these medications have limitations. Some can lead to drug dependence in the long term, while others can cause unwanted side effects, such as rebound headaches or gastric ulceration. So their use should be carefully managed.
Michelle adds, ‘The most important advice I would give to a migraine sufferer is to identify and reduce or avoid the trigger(s) that cause migraines. Commonly reported triggers include certain foods, environmental triggers such as loud noises or weather changes, and behavioural-physiologic triggers such as insufficient sleep or stress.’ She recommends keeping a daily diary to document migraines and possible triggers. ‘This is an effective, inexpensive tool to follow the course of the disorder and receive the appropriate treatment.’
The information is shared on condition that readers will make their own determination, including seeking advice from a healthcare professional. E&OE. Life Healthcare Group Ltd does not accept any responsibility for any loss or damage suffered by the reader as a result of the information provided.

